Human papillomavirus: characteristics and associated diseases.
Summary of the characteristics of human papillomavirus, explaining its degree of danger.
Human papillomavirus (HPV) is an umbrella term for various groups of DNA viruses belonging to the family Papillomaviridae. According to various professional sources, there are more than 200 types of HPV, of which about 40 are correlated with infections in the genital area and sexual contact.
We are dealing with a viral family that can cause anything from a slight self-resolving wart in time to cervical Cancer in women. Of course, it is impressive to know that within the same family, different members can generate such diverse problems in humans. Moreover, of the 16 existing genera, only 5 affect our species, the rest being pathogenic agents for other animals.
To make things more interesting, it is estimated that more than 90% of sexually active people have HPV at some point in their lives, meaning that virtually every adult is infected. Incredible, isn't it? Here's everything you need to know about this multifaceted viral family.
What is human papillomavirus? From wart to cancer
Human papillomavirus infections occur worldwide, i.e. there is no country, ethnicity, age or sex immune to this infectious agent. Before launching into the exciting epidemiology of the disease, let us briefly describe the causative agent.
Small but thuggish
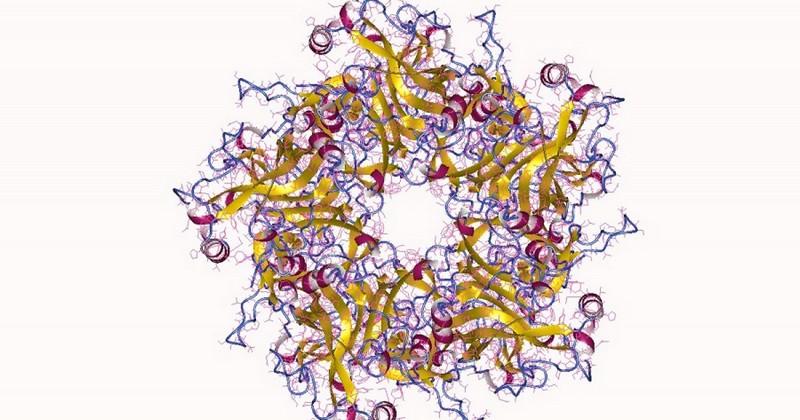
As mentioned above, the term HPV does not refer to a specific viral species, but to an entire family. Even so, all pathogens included in this grouping share a number of characteristics. For example, they are all double-stranded DNA viruses (i.e. their genome is composed of DNA) with about 8,000 base pairs. The genome of these pathogens can be divided into an early (E) region, a late (L) region and a control region..
In terms of morphological structure, they lack an envelope and have a diameter of about 50 nanometers. It is an extremely simple virus, since a single protein (L1) is sufficient for the complete formation of the capsid that protects the genetic information of the pathogen. There is another much less abundant coat protein (L2), which still has functions that have not yet been fully described.
Because the capsid-forming proteins of all papillomaviruses are antigenically similar, these viruses cannot be categorized into distinct serotypes (i.e., according to cell surface antigens). Therefore, the subtypes described are based on the antigens on the cell surface, subtypes described are based on differences in the DNA double helix (e.g., HPV 16 or HPV 16). (e.g. HPV 16 or HPV 1). It should be noted that for a particular virus to be considered a subtype, the genetic difference with respect to its peers must be 2 to 5%.
A diverse pathogenesis
Once we have made a concrete mental picture of this problematic pathogen, it is essential that we divide the human papillomaviruses according to their dangerousness, i.e. whether they are oncogenic or not.that is, whether they are oncogenic or not. Let's get down to it.
1. Cutaneous HPV
If any of the readers, upon observing a wart on their body, believe that they are facing a skin lesion due to trauma, they are mistaken. It is surprising to learn that warts are formed by HPV infection, albeit of completely different subtypes than those that cause cancer.HPV infection, albeit of completely different subtypes than those that cause cervical cancer (in most cases).
Thus, we can see common warts, flat warts, and warts caused by HPV, we can see common, flat, palmoplantar, etc. warts. These respond to various papillomaviruses: HPV 1, HPV 2, HPV 3, HPV 4, HPV 26, HPV 41 and a very long list of numerical concatenations. In the vast majority of cases they are ubiquitous and asymptomatic infections, i.e. they are widely distributed and do not cause any harm, as they resolve by themselves over time.
This type of infection can affect up to 10% of children and adolescents, and the virus penetrates the epidermis and spreads by autoinoculation, causing this characteristic formation that can last up to 18 months after primary infection. Of course, in the world of warts, there is nothing to worry about.
2. Genital HPV
Here things get more complicated. It should be noted that the vast majority of genital HPV infections in young women are temporary and have little long-term significance.. To the relief of any reader, 70% of infections go away on their own within a year, and 90% within two years. Still, it is necessary to report the outlier, which is that this group includes potentially oncogenic HPVs.
Unfortunately, HPV 16 and HPV 18 subtypes are responsible for 70% of cervical cancers and precancerous lesions in the cervix. Although in most cases these types of infections are self-resolving, in a small percentage of the population they develop into permanent conditions, which can turn normal cells into precancerous lesions or cancer.
Of the more than 150 types of human papillomaviruses in existence, about 14 are considered oncogenic.Unfortunately, HPV infection is the most common STI worldwide. As a result, an estimated 311,000 women died in 2018 as a direct result of the infection. More than 85 % of the deaths occurred in low- and middle-income countries. We are not only moving into the female gender from a binary point of view, as oncogenic HPVs have also been correlated with penile, anal, head and neck cancers.
It should be noted that not all genital infection-forming HPVs are high risk. For example, HPVs 6 and 11 are correlated with the majority of warts in the sexual organs, but are considered to be of low oncologic risk, since their probability of generating cancer in humans is low.
A cosmopolitan distribution
It is virtually impossible to cover the symptomatology and treatment of human papillomavirus.The existing subtypes manifest themselves in different ways and the methods of transmission are diverse (although they are united in the production of warts, for example).
We find it much more interesting, in this case, to make a global map of this viral family and contextualize it from a population point of view.. Let's get down to it:
- HPV 16 (unfortunately, high-risk) is the most common subtype worldwide, except for Indonesia and Algeria, where HPV 18 reigns.
- The highest prevalence of high-risk oncogenic HPV types 16, 18, 31, 33, 35, 45, 51, 52, 58, 59 is found in Africa and Latin America.
- HPV 45 has a high incidence in West Africa.
- Subtypes 33, 39 and 59 are concentrated in Central and South America.
- About 6.2 million U.S. adults or adolescents aged 15-44 years were infected with genital HPV in 2000.
- At any given time and region, about 30% of women aged 14-59 years are infected with at least one type of HPV.
From a purely epidemiological point of view, we are dealing with a viral family of a fascinating nature, as its distribution is cosmopolitan and does not understand ethnicity, age or gender. Fortunately most of the infections are harmless, otherwise we would be facingOtherwise we would be facing a serious global problem that would be difficult to eradicate.
It should be noted that, due to their exaggerated prevalence, highly effective vaccines have been developed against HPV subtypes 16 and 18. It is recommended that women be vaccinated before becoming sexually active, as this preventive treatment is of little benefit to a person who is already infected.
Summary
As we have seen, we are dealing with a fascinating (but relatively dangerous) viral family, with so much information and infective dynamics that a book could be written about it without any difficulty. If there is one thing we want to make clear, it is that there are many, many subtypes of human papillomavirus, most of them harmless, but a few (at least 14) of high riskbecause of their potential to generate cancer in the individual.
When any reader analyzes a wart from now on, he or she will know the truth behind it: a harmless infection. Papillomaviruses are a multifaceted and problematic family of pathogens, but they are still fascinating viruses from an epidemiological point of view.
Bibliographic references:
- What is HPV? Plannedparenthood.org. Retrieved September 16 from https://www.plannedparenthood.org/es/temas-de-salud/enfermedades-de-transmision-sexual-ets/vph.
- Human papillomavirus and cancer, Cancer.net. Retrieved Sept. 16 from https://www.cancer.net/es/desplazarse-por-atenci%C3%B3n-del-c%C3%A1ncer/prevenci%C3%B3n-y-vida-saludable/el-virus-del-papiloma-humano-vph-y-el-c%C3%A1ncer.
- Papillomavirus infection, Centers for Disease Control and Prevention. Retrieved Sept. 16 from https://www.cdc.gov/std/spanish/vph/stdfact-hpv-s.htm.
- Human papillomavirus (HPV) and cervical cancer, World Health Organization (WHO). Retrieved September 16, from https://www.who.int/es/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer
- Rivera, R., Aguilera, J., & Larraín, A. (2002). Epidemiology of human papillomavirus (HPV). Revista chilena de obstetricia y ginecología, 67(6), 501-506.
(Updated at Apr 12 / 2024)