Metachromatic leukodystrophy - symptoms, causes and treatment
This neurodegenerative disease of genetic origin causes cognitive, motor and speech symptoms.
Metachromatic leukodystrophy is an inherited, neurodegenerative disease It affects the white matter of the nervous system and is caused by an enzyme deficiency. This disorder causes severe effects on neurocognitive and motor functions.
In this article we explain what this disease consists of and what are its main characteristics, its variants, the causes that provoke it, its symptoms and the indicated treatment.
Metachromatic leukodystrophy: definition and characteristics.
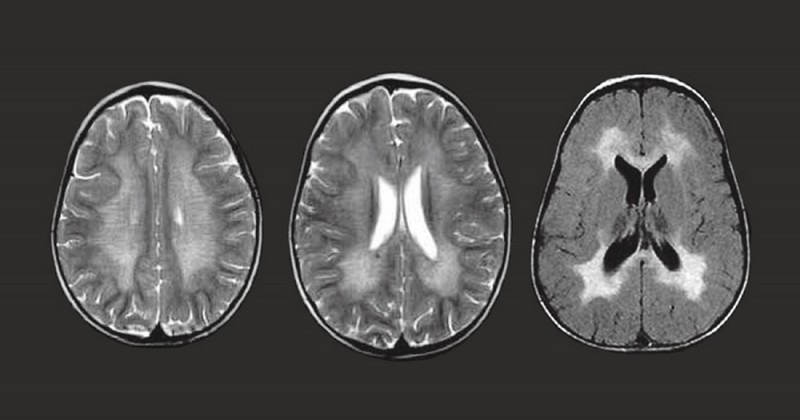
The metachromatic leukodystrophy is a rare hereditary disorder, belonging to the group of the diseases by lysosomal deposit, characterized by accumulation of sulfatides in cells, especially in the nervous system.. This accumulation causes progressive destruction of the white matter of the brain, formed by nerve fibers covered with myelin.
Myelin is a substance that coats the axons of nerve cells and its function is to increase the speed of transmission of nerve impulses. Its deterioration or destruction has devastating effects on the patient's cognitive functions and motor skills.
The main characteristic of the leukodystrophies that belong to the group of lysosomal diseases, such as metachromatic leukodystrophy, is malfunction of the enzymes of the lysosome, a cellular structure containing numerous enzymes.This is a cellular structure containing numerous enzymes whose function is to degrade and recycle intracellular material (of external and internal origin), in a process known as cellular digestion.
This disease can have its onset in childhood, adolescence or adulthood, and is transmitted in an autosomal recessive pattern; that is, the person has to inherit two copies of the genetic mutation (one from each parent) to have the disease. The incidence of metachromatic leukodystrophy at birth is estimated at 1 case per 45,000 children, and represents about 20% of all leukodystrophies.
Causes
The causes of metachromatic leukodystrophy are genetic; specifically, mutations in the ARSA and PSAP genes appear to be responsible for a deficiency of the enzyme arylsulfatase A (ARSA), which is responsible for the development of the arylsulfatase A (ARSA) enzyme.which is responsible for breaking down sulfatides and other fats.
Rarely, a deficiency of saposin activator protein B (Sap B), which helps the enzyme ARSA to break down these fats, could also be another possible cause of the disease. The accumulation of sulfatides in the cells is due to a malfunction of the common work of ARSA and Sap B in degrading these fatty compounds.
Types (and symptoms of each)
There are three types of metachromatic leukodystrophy, which are classified according to the age of onset of the disease, each with its distinctive symptoms. Let us see what they are:
1. late infantile form.
This form of metachromatic leukodystrophy is the most common. is the most common and accounts for about 50-60% of cases.. It usually originates in the first two years of life and the children, after a period of relative normalcy, gradually lose acquired skills and suffer from mobility problems (abnormal or erratic movements) and muscle weakness (problems walking or crawling).
These children are often diagnosed with cerebral palsy due to mobility impairment.. As the disease progresses, muscle tone decreases to a state of absolute rigidity, speech problems become increasingly evident, and difficulties in fine motor skills appear.
Eventually, the child loses the ability to think, understand and interact with others. The mortality rate is high and children often do not survive beyond infancy.
Juvenile form
This form of metachromatic leukodystrophy is the second most common (about 20-30% of cases). It usually begins between the age of 2 or 3 years and adolescence. The first symptoms of the disease have to do with problems with fine motor skills and concentration.. Behavioral disturbances may also occur during the academic year.
These children may also have difficulty interacting with their peers and sometimes a possible diagnosis of schizophrenia or depression is suspected. In the early stages, they can barely move, coordinate, walk or develop speech properly.
As symptoms progress, other neurological signs other neurological signs appear, such as involuntary flexion, tremors, muscle rigidity with eventual loss of gait.. Progression of the disease is slower than in the late infantile variant and affected children may survive for about 20 years after diagnosis.
3. Adult form
The adult form is the least common variant of metachromatic leukodystrophy (15-20% of cases). The first symptoms appear during adolescence or later and are reflected in poor school or work performance, with a progressive decline in cognitive abilities and behavioral problems. progressive decline in cognitive abilities and behavioral problems.. The affected person may also suffer from psychiatric symptoms such as delusions or hallucinations.
In addition, patients show motor clumsiness and may become incontinent. There is also paralysis of the arms and legs, which develops progressively. Occasionally, seizures may also occur. In the later stages of the disease, affected individuals may In the final stages of the disease, affected individuals may reach a vegetative state.
In the late stages of the disease, affected individuals may reach a vegetative state, if one has this variant, one can survive for 20 to 30 years after diagnosis.. During this time there may be some periods of relative stability, as opposed to other periods of greater instability.
Treatment
Although there is no definitive cure for metachromatic leukodystrophy there is still no definitive cure for metachromatic leukodystrophy, the usual treatments for this disease includeThe usual treatments for this disease include:
1. symptomatic and supportive treatment 2.
It is based on antiepileptic drugs, muscle relaxants, physical therapy for the improvement of muscle function and mobility, cognitive stimulation and support to relatives to anticipate future decisions on the acquisition of technical aids (walkers, wheelchairs, feeding tubes, etc.).
2. Hematopoietic stem cell or bone marrow transplantation
Here use is made of healthy stem cells obtained from the Blood or bone marrow of a donor and injected into the patient.. This procedure is not recommended in the late infantile variant, but may be potentially beneficial in patients with the juvenile and adult form, especially in the early stages of the disease.
3. Enzyme replacement therapy
Although this therapy is still under investigation and clinical trials are ongoing, animal studies suggest that it may reduce sulfatide accumulation and lead to functional improvement in the patient.
4. Gene therapy
Consists of replacing defective genes with healthy copies. may be a treatment in the future and is being worked on and researched..
5. Injection of adeno-associated viral vectors
This method consists of injecting a genetically modified virus containing a normal copy of the ARSA gene into the brain, so that it can "infect" the cells and incorporate the gene into them. This would theoretically restore enzyme levels. It has been successful in animal models and clinical trials are being carried out in several countries.
Bibliographic references:
- Alvarez-Pabón, Y., Lozano-Jiménez, J. F., Lizio-Miele, D., Katyna, G., & Contreras-García, G. A. (2019). Late infantile metachromatic metachromatic leukodystrophy: A case report. Archivos argentinos de pediatría, 117(1), e52-e55.
- Gieselmann, V., & Krägeloh-Mann, I. (2010). Metachromatic leukodystrophy-an update. Neuropediatrics, 41(01), 1-6.
(Updated at Apr 13 / 2024)