HIV-associated dementia: symptoms, stages and treatment
This type of dementia is associated with the effects of immune system degradation.
HIV infection and AIDS are still a global pandemic today. Although more and more prevention policies are being put in place and the pharmacotherapy that exists today means that it has gone from being a death sentence in a few years to being a chronic disease in a large number of cases, the fact remains that it is still a major problem in much of the world that requires much more research in order to try to find a cure.
Although most people know what HIV and AIDS are (although they are often identified although they are not exactly the same thing) and their effects in terms of weakening the immune system, less well known is the fact that in some cases it can cause, in advanced stages, a type of dementia. This is HIV-associated dementiawhich we are going to talk about in this article.
HIV and AIDS: Basic definition
Before discussing what HIV-associated dementia is, it is necessary to briefly review what HIV and AIDS are (and to mention that they are not synonymous and that HIV does not necessarily imply the development of AIDS).
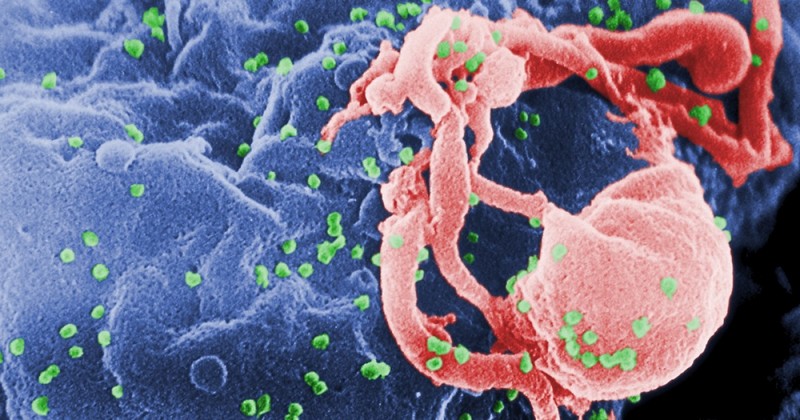
The acronym HIV refers to the Human Immunodeficiency Virus, a retrovirus whose action affects and attacks the human immune system, especially affecting CD4+ T lymphocytes (causing, among other things, the intestinal mucosal cells that generate them to deteriorate and disappear) and causing a progressive deterioration of this system as the virus multiplies.
AIDS would refer to the Acquired Immunodeficiency Syndrome, in which the immune system is so damaged that it is no longer able to respond to infections and pathogens efficiently. and pathogens efficiently. This is an advanced stage of HIV infection, but it may not appear at all. HIV infection may not progress to this point.
The appearance of neurological symptoms during HIV infection or during AIDS is not unknown, and some nervous alterations (with symptoms ranging from hypotonia, loss of sensitivity, paresthesias, physical slowing, behavioral changes or mental slowing, among others) may appear at different points in the system at any time during the infection.
In some cases cognitive impairment may occur as a result of HIV infection or due to opportunistic infections. or derived from opportunistic infections. The presence of cognitive impairment is generally more typical of advanced stages, usually already during AIDS. Minimal cognitive impairment without serious complications may occur, but a much more important complication, HIV-associated dementia, may also occur.
HIV-associated dementia: basic characteristics and symptoms
HIV-associated dementia, or dementia-AIDS complex, is a neurological disorder characterized by progressive neurodegeneration that causes progressive loss of cognitive and motor faculties and abilities resulting from the involvement of HIV infection. The involvement of the immune system and the action of the virus eventually damage the nervous system, especially affecting areas such as the basal ganglia and frontal lobe.
The mechanism by which they do so is not fully known, although it is hypothesized that the following may be involved the release of neurotoxins and cytokines by infected lymphocytes, especially in the cerebrospinal fluid, which in turn would cause an excessive increase in the release of glutamate leading to excitotoxicityThis in turn would cause an excessive increase in the release of glutamate which would generate excitotoxicity, damaging neurons. The involvement of the dopaminergic system is also suspected given that the most damaged areas initially correspond to pathways linked to this neurotransmitter and the symptoms resemble other dementias in which there are alterations in this.
We are dealing with a dementia of insidious onset but of rapid evolution in which capacities derived from neurological involvement are lost, with a profile that debuts in a frontosubcortical manner (i.e., the alteration would start in the internal parts of the brain located in the frontal area, and not in the cortex). We would be talking about a primary type of dementia, characterized by the presence of cognitive impairment, behavioral changes and motor dysfunction. The type of symptomatology is similar to the dementia that can appear with Parkinson's disease or Huntington's chorea.
It usually begins with a loss of the ability to coordinate different tasks, as well as a slowingIt usually begins with a loss of the ability to coordinate different tasks, as well as a mental slowing or bradypsychia (which is one of the most characteristic symptoms), although at first the capacity for reasoning and planning remains preserved. As the disease progresses, memory and concentration problems appear, as well as visuospatial and visuoconstructive deficits, depressive symptoms such as apathy and motor slowing. Reading and problem solving are also altered.
In addition, it is common to see apathy and loss of spontaneityThe patient may have delusions and hallucinations (especially in the final stages), as well as confusion and disorientation, language disturbances and progressive isolation. Autobiographical memory may be impaired, but this is not an essential criterion. Verbal memory is usually affected at the level of evocation, as well as alterations in procedural memory (how to do things, such as walking or cycling).
Not only are cognitive functions affected, but also neurological alterations such as hyperreflexia, muscular hypertension, tremors and ataxias, convulsions and incontinence. Alterations in eye movement may appear.
Another point to be especially noted is that the onset of this type of dementia usually implies the existence of AIDS, being characteristic of the final stages of this syndrome. Unfortunately, the evolution of this disorder is surprisingly rapid: the subject loses capacities at great speed until his death, which usually occurs about six months after the onset of symptoms if he does not undergo any treatment.
Finally, it should be noted that children can also develop this dementia, with maturational developmental delays and microcephaly appearing in addition to the above symptoms.
Stages of HIV-associated dementia
HIV-associated dementia usually develops and progresses rapidly over time. However, it is possible to distinguish between different phases or stages of evolution of this type of dementia.
Stage 0
Stage 0 is the time when the HIV-infected person does not yet have any symptoms. does not yet show any neurodegenerative symptoms.. The subject would maintain his cognitive and motor abilities, being able to perform daily activities normally.
Stage 0.5
This is the point at which some abnormalities begin to appear. Alterations in some activity of daily living may be detected, or some type of symptom may appear, such as some type of symptom such as a slight slowing down may appear although there are no difficulties in daily life.
Stage 1
In this stage already begin to manifest alterations in the patient's abilities. Activities of daily living and neurological examinations reflect mild impairment. The subject is able to cope with most activities except those that are more demanding. He does not need help to move, although signs of cognitive and motor impairment appear.
Stage 2
In this stage dementia is in a moderate stage. Although he can perform basic activities, loses the ability to work and begins to need external aids to get around.. Clear neurological alterations are observed.
Stage 3
Severe dementia. The subject is no longer able to understand complex situations and conversations, and/or requires help to move around at all times. Slowing down is common.
Stage 4
The final and most severe stage, the person only maintains the most basic abilities, it is not possible to perform any type of neuropsychological evaluation.. Paraplegia and incontinence appear, as well as mutism. The person is practically in a vegetative state, until death.
Treatment of this rare dementia
The treatment of this type of dementia requires a rapid response in the form of treatment, since the symptomatology evolves and progresses rapidly. As with other dementias, there is no curative treatment, but it is possible to prolong functionality and improve the patient's quality of life. Treating this dementia is complex. First of all, it must be borne in mind that dementia is caused by the effects of the immunodeficiency virus. caused by the effects of the human immunodeficiency virus on the brain.It is therefore imperative to reduce and inhibit as much as possible the viral load in the cerebrospinal fluid.
Pharmacology
Although there is no specific pharmacological treatment for this type of dementia, it is necessary to take into account that the usual treatment with antiretroviral drugs will continue to be necessary, although it will not be sufficient to stop the progression of dementia. The use of those that can better penetrate the blood-brain barrier is recommended. Several antiretroviral drugs (at least two or three) are used in combination, this treatment being known as retroviral combination therapy or Targa.
One of the most widely used drugs with the most evidence in reducing the incidence of this dementia is zidovudine, generally in combination with other antiretroviral drugs. zidovudine, generally in combination with other antiretrovirals (two, three or more). (two, three or more). Also azidothymidine, which seems to improve neuropsychological performance and serve as a prophylactic against the onset of this dementia (which has decreased over time).
Neuroprotectants such as calcium channel blockers, NMDA glutamate receptor antagonists and inhibitors of oxygen free radical production are also recommended. Selegiline, an irreversible MAOIselegiline, an irreversible MAOI, has been found useful in this regard, as has nimodipine. In a complementary manner, the use of psychostimulants, anxiolytics, antipsychotics and other drugs is also recommended in order to reduce the hallucinatory, anxious, depressive, manic or other disorders that may arise.
Other aspects to work on and take into account
Beyond medical and pharmacological treatmentIt is very useful for the patient to be in a protected environment that provides support, as well as the presence of aids that facilitate orientation and stability. Following a routine greatly facilitates the person to maintain a certain sense of security and facilitates the preservation of memory, being also necessary to be notified in advance of possible changes.
Physiotherapy and occupational therapy can facilitate the maintenance of abilities for a longer period of time and promote a certain degree of autonomy. Psychological therapy can be useful, especially with regard to the expression of fears and doubts by both the subject and his close environment.
Although dementia will reappear over time and will progressively evolve, it is certain that the treatment can promote a really considerable improvement and prolong the maintenance of and prolong the maintenance of the patient's abilities and autonomy.
Bibliographical references:
- Lopez, O.L. and Becker, J.T. (2013). Acquired Immunodeficiency Syndrome-Associated Dementia and the Dopaminergic Hypothesis. Behavioral neurology and dementias. Spanish Society of Neurology.
- Custodio, N.; Escobar, J. and Altamirano, J. (2006). Dementia associated with human immunodeficiency virus type 1 infection. Annals of the Faculty of Medicine; 67 (3). Universidad Nacional Mayor de San Marcos.
(Updated at Apr 13 / 2024)