Urinary tract infections – symptoms, risks, treatment

The urinary tract (UT) is sterile, i.e. it doesn’t contain any bacteria. If any bacteria, viruses, or fungi are present in it, then we can talk about a urinary tract infection (UTI). The infection induces inflammation and unpleasant symptoms that make patients seek medical advice.
Urinary tract infections – short info
To better understand the disease, for a patient it is better to understand the functions of the genitourinary system parts. The kidneys are located by the sides of the spinal column. They cleanse the blood and regulate the chemical balance in the organism.
The kidneys filter out ballast substances from the blood and plasma which are accumulated in urine to be washed out. These substances include products of nitrogen metabolism, toxins and medicines, foreign elements, and inorganic compounds. Urine slowly flows down the ureters into the bladder.
When enough urine has accumulated fills it, a person feels the urge to urinate. When urinating, urine descends through the urethra and is washed out of the body.
The UT is divided into upper and lower and so are the UTIs:
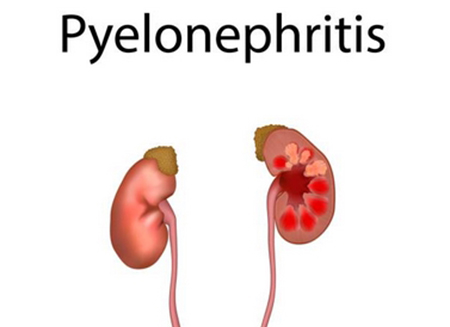
- Upper UTI: pyelonephritis (kidney disease);
- Lower UTIs: cystitis (bladder disease), urethritis (urethra disease), and prostatitis (prostate disease).
Women develop UTIs 50 times more frequently than men. They predominantly have cystitis and pyelonephritis. In men, the most frequent diseases are prostatitis and urethritis.
UTIs can be uncomplicated and complicated. UTIs are deemed uncomplicated if they develop in adult women without congenital defects of the UT.
They are deemed complicated if these criteria are present:
- Congenital disorders of the UT;
- Presence of a secondary disease that aggravates UTI, such as diabetes or immunodeficiency;
- Age under 18 years old;
- Pregnancy.
What causes UTIs?

Despite the common ingress of bacteria from the colon (improper hygiene, migration of microorganisms), local defense mechanisms keep the UT absolutely clean. For instance, the main defense force is urination that washes out all pathogens. Auxiliary mechanisms - acidic urine reaction, vesicoureteral valve, mucous membranes, and local immunity.
Nevertheless, in the overwhelming majority of cases, UTIs occur on the base of bacteria from the colon. The bacteria can also get into the UT through the blood from another organ that is infected.
In the remaining 5% of cases, infectious diseases are caused by pathogenic fungi (mainly from the Candida genus). Even less often - mycobacterium tuberculosis, parasites (filariasis, schistosomiasis, leishmaniasis, trichomoniasis, and malaria) and viruses. Fungi and mycobacteria infect people with weak immunity, birth defects of the UT, and diabetes.
The risk factors for UTIs are sexual contact and improper hygiene of the genitourinary organs.
Risk factors:
- Unprotected sex or a new sex partner;
- Use of antibiotics in high doses or for an extended period of time;
- Use of a diaphragm or spermicide as birth control;
- UTI in a first-degree relative;
- A previous UTI.
The risk raise related to spermicides or antibacterial drugs is explained by the fact that the vaginal environment changes and additional conditions are created for the multiplication of Escherichia coli, i.e. intestinal bacteria.
Other risk factors include congenital anomalies causing vesicoureteral reflux (the urine spontaneously flows back). This is a rare occurrence in adults as it is usually diagnosed in babies and treated.
A person can also acquire UTI as a result of surgery or medical instrumental procedures: catheterization, cystoscopy or wall placement.
Symptoms of a UTI

UTI causes urethritis, cystitis, acute urethral syndrome, and acute pyelonephritis.
Urethritis symptoms in men:
- Difficulty urinating;
- Purulent, slimy, or whitish discharge from the UT.
Cystitis manifestations:
- Frequent needs to urinate;
- False needs to urinate;
- Burning sensation, itching, and pain during urination;
- Urine is usually cloudy, often reddish;
- Nighttime urination with pain above the pubis;
- Fever may occur with a temperature of 37.1 to 38.0 degrees Celsius;
- Rapid and sudden onset of symptoms.
Symptoms of acute pyelonephritis:
- Back pain from an infected kidney; usually it is aching and dull pains, sometimes the pain can be cramping;
- Body temperature from 38 to 40 degrees;
- General weakness;
- Headaches;
- Nausea and vomiting;
- No appetite;
- Irritability.
There is a specific infectious disease - asymptomatic bacteriuria. It proceeds without signs and symptoms, but if an examination is carried out, then bacteria are found.
Why do women get UTIs more frequently?

This is due to the female genitourinary system anatomy. The women's urethra is shorter than the men's, so bacteria need to travel a shorter distance to enter the organs of the UT.
The second factor is the proximity of the urethra and colon. Bacteria easily migrates from the colon to the urethra. To minimize the risk, women should wipe from front to back and teach girls to do so from an early age to prevent UTIs. The third factor is having sex: the microflora of the penis or vagina can also penetrate into the urethra.
The vaginal diaphragm can raise the likelihood of infection because it makes fully emptying the bladder difficult. This troubles the urine function, i.e. excretion of the bacteria. Bacterial cultures will begin to grow in it - inflammation will begin.
Besides, UTIs in women can be promoted by alteration of the vaginal bacterial flora due to spermicides and taking antibiotics. Avoid these factors if applicable and use other methods of contraception.
In menopause, the risk of UTIs also grows. Usually, estrogen-based medications solve the problem, but consult your gynecologist before using them.
How are UTIs diagnosed?
A urinalysis and urine culture are the key tests to diagnose UTIs. If an STI is suspected, a swab of the urethra is made. Keep in mind that different urine tests require different portions of urine. Make sure to clarify with your doctor how you should collect the urine for the test.
Can UTIs be prevented?

Yes, they are preventable. To do this, following these tips:
- Drink more water: drink at least 1.5 liters of liquid a day; cranberry juice is also advised to be consumed for prevention; but, if you are taking warfarin, you should talk to your doctor before drinking it;
- Do not hold back the urge to go to the toilet and teach your kids to go to the toilet once they feel the need;
- After urinating, wipe the external genitals from front to back, and not vice versa, teach your kids the same;
- The best natural prevention of infection after sex is to urinate;
- Use lubricant before or during sex; do not allow the vaginal mucosa to remain dry and irritated;
- Wear loose cotton underwear;
- Uncircumcised men need to regularly wash the penis and especially the foreskin: smegma accumulates under it, which is a good breeding ground for bacteria.
If these preventative measures are ineffective, your doctor will prescribe prophylactic antibiotics.
Trial continuous prophylaxis lasts 6 months. If a UTI occurs 6 months after taking the medication, preventive treatment is extended to 2 years. The medication should be chosen based on the pathogen, your immunity, and resistance.
If a UTI is associated with sex, postcoital prophylaxis is used. One dose of medicine is sufficient to prevent infection.
Treatment of UTIs

Most of the time, antibiotics therapy is prescribed and less often surgery (if abscesses or obstruction have developed). The most frequently used medicines are Cefaclor, Amoxiclav, Augmentin, and others.
The goal of therapy is to completely free the UT from bacteria and make it sterile again.
The doctor chooses antibiotics contingent on your allergic history, culture, and drug resistance. In most cases, only several days of antibiotics use are sufficient to treat a UTI. After 2–3 days, the manifestations of the disease begin to subside. When you feel better, you should continue taking your medication: if you miss a few doses of the pills, the treatment will lose its effectiveness.
Complications of UTI

A urinary tract infection can cause kidney complications.
- Multiple kidney abscesses occur when the infection enters the kidney through the bloodstream. Small purulent accumulations form in the kidney cortex, which eventually merge into one large abscess. Sometimes pus erupts into the urinary tract. In this case, it enters the urine. It mostly happens in individuals with aggravating factors: diabetes or injecting drug addicts.
- A perinephric abscess is a collection of pus between the fascia of the kidney and its capsule. It occurs as a complication of pyelonephritis. In 25% of cases, it develops in individuals with diabetes mellitus. It manifests itself in severe pain in the affected kidney and high fever.
- Papillary necrosis occurs when the infection rises to the kidneys. The disease is distinguished by the damage of the renal papilla and manifests by severe renal colic. Most often it develops in people with diabetes mellitus.
- Chronic pyelonephritis occurs due to recurrent acute pyelonephritis. It is common in people with defects in the anatomy of the UT. The disease may cause kidney failure.
- Acute prostatitis occurs due to urethra infection. It is distinguished by a rapid increase in symptoms: the body temperature rises, there is severe pain in the pelvis, and it is difficult and painful to urinate.
Post by: Jacob Hansen, General healthcare practitioner, National health centre, Stavanger, Norway
(Updated at Apr 15 / 2024)
Ceclor articles:
Some of the trademarks used in this Web Site appear for identification purposes only.
All orders are reviewed by a licensed physician and pharmacist before being dispensed and shipped.
The statements contained herein are not intended to diagnose, treat, cure or prevent disease. The statements are for informational purposes only and is it not meant to replace the services or recommendations of a physician or qualified health care practitioner. If you have questions about the drugs you are taking, check with your doctor, nurse, or pharmacist.