Urinary tract infections – symptoms, treatment, prevention


What is a urinary tract infection?
Urinary tract infection (UTI) is characterized by the presence of microorganisms in the urinary tract above the sphincter of the bladder, which are normally sterile.
Significant bacteriuria (presence of bacteria in urine) is the number of living bacteria (so-called colony-forming units - CFU) of one strain in ml of urine, indicating an UTI. Depending on the form of the IC, these are:
1) ≥103 CFU / mL in a woman with symptoms of bladder inflammation in a midstream urine sample;
2) ≥104 CFU / ml in a woman with symptoms of acute pyelonephritis (AP) in a midstream urine sample;
3) ≥105 CFU / ml in the case of complicated UTI in a midstream urine sample;
4) ≥102 CFU / ml in a portion of urine sampled by a single insertion of a catheter into the bladder;
5) any number of CFU in urine obtained by suprapubic puncture of the bladder.
Short information about urinary tract infections
Asymptomatic bacteriuria is significant bacteriuria (≥105 CFU/ml in the midstream urine or ≥102 CFU/ml in the urine sample collected by a single insertion of a catheter into the bladder) in a person without subjective and objective symptoms of UTI. The presence of leukocyturia in a patient without clinical symptoms is not sufficient to diagnose an UTI.
Complicated UTIs are:
1) Any UTI in a man;
2) An UTI in a woman with an anatomical or functional disorder that prevents the outflow of urine, or with a decrease in the level of systemic or local defense mechanisms;
3) An UTI caused by atypical microorganisms.
Uncomplicated UTI occurs in women with a normal genitourinary system and without disturbances in local and systemic defense mechanisms (that is, without risk factors for UTI, see below) and is caused by microorganisms typical of UTI.
Recurrent UTI is a repeated UTI that occurs after antimicrobial therapy, due to the survival in the urinary tract of the microorganism that caused the primary UTI. In practice, a recurrence of an UTI is diagnosed if its symptoms have occurred <2 weeks after the end of treatment for a previous UTI, and the etiological factor is the same microorganism.
Repeated UTI (reinfection) is an UTI caused by a microorganism coming from outside the urinary system, which is a new etiological factor. In practice, recurrent UTI is diagnosed if symptoms have occurred after 2 weeks after the end of the previous UTI treatment, even if the etiological factor is the same microorganism.
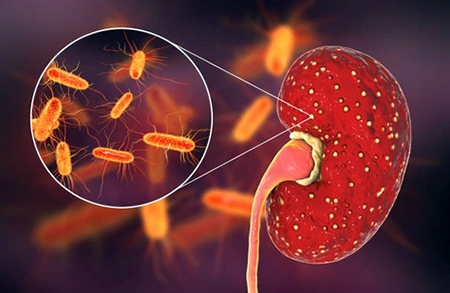
Under normal conditions, the urinary tract is sterile, with the exception of the distal urethra, which is inhabited mainly by saprophytic coagulase-negative staphylococci (e.g. Staphylococcus epidermidis), vaginal sticks (Haemophilus vaginalis), non-hemolytic bacteria streptococci and lactobacilli. Pathogenic microorganisms colonize the urinary system mainly in the ascending route. The first stage in the development of UTI ascending is the colonization of the urethra orifice by uropathogenic bacteria. This more often occurs in women in whom the vestibule of the vagina is the reservoir of uropathogenic microorganisms; the distance from the mouth of the urethra to the anus is also smaller.
The next stage is the penetration of microorganisms into the bladder in women, often during intercourse. In people with effective defense mechanisms, colonization ends at the level of the bladder. The likelihood of a kidney infection increases as the bacteria remain in the bladder. Hematogenous and lymphogenous infections account for ≈2% of all UTI, but these are most often severe cases occurring in patients in severe clinical condition with weakened immunity.
Risk factors for complicated UTI:

- Urinary retention;
- Urolithiasis (the formation of stony concretions in the bladder or urinary tract);
- Vesicoureteral reflux (the flow of urine goes the wrong way);
- A catheter in the bladder;
- Diabetes mellitus (especially decompensated),
- Old age;
- Pregnancy and childbirth;
- Hospitalization for other reasons.
Etiological factors (what causes the diseases):
1) Bacteria:
a) Uncomplicated and recurrent cystitis - Escherichia coli (70–95% of cases), Staphylococcus saprophyticus (5–10%, mainly in sexually active women), Proteus mirabilis, Klebsiella spp., Enterococcus spp. and others (≤5%);
b) Acute uncomplicated pyelonephritis (AUP). The same pathogens but greater participation of E. coli without S. saprophyticus;
c) Complicated UTI - E. coli (≤50%), more often than in uncomplicated UTI, bacteria from the species Enterococcus (20%), Klebsiella (10-15%), Pseudomonas (≈10%), P. mirabilis and infections with more than one microorganism;
d) Asymptomatic bacteriuria - in women most often E. coli; in patients with a long-term catheter, several microorganisms are usually present in the bladder, often including Pseudomonas spp. and urease-positive bacteria (eg Proteus spp.);
2) Microorganisms not detected by standard methods - Chlamydia trachomatis, gonococci (Neisseria gonorrhoeae), viruses (mainly Herpes simplex); almost exclusively sexually transmitted, cause up to 30% of lower urinary tract infections in sexually active women;
3) Fungi - most often Candida albicans and other species of the genus Candida, Cryptococcus neoformans and Aspergillus; are the cause of ≈5% of complicated UTI. Fungal UTI most often occurs in diabetic patients receiving antibiotics, with a catheter in the bladder, in patients after manipulations on the urinary tract, primarily in patients receiving immunosuppressants. Yeast can be found in urine without causing an UTI.
Clinical picture and natural dynamics

Depending on the natural course, as well as the necessary diagnostic and therapeutic procedures, there are:
1) Acute cystitis in women. Most often, dysuria, pollakiuria (increased urination frequency) and pain in the suprapubic region, sometimes urinary incontinence, and hematuria (in ≈40% of cases), as well as sensitivity to palpation in the suprapubic region. Revealed leukocyturia and bacteriuria> 105 CFU / ml (in some patients 102-104 CFU / ml). Untreated cystitis lasts from several days to several tens of days. Imaging studies and urine culture are usually performed only when symptoms persist during treatment or recur within 1–4 weeks.
Treatment
1. First-line drugs: fosfomycin trometamol orally 2.0 g or 3.0 g (depending on body weight) once in a glass of water or Nitrofurantoin 100 mg 2 × a day for 3-5 days, cotrimoxazole 960 mg 2 × daily for 3 days, trimethoprim 100 mg 2 × daily within 3 days. If E. coli resistance to cotrimoxazole > 20% is detected in the regioe, use another first-choice drug instead of cotrimoxazole and trimethoprim, fluoroquinolone (for 3 days: ciprofloxacin 250 mg 2 × daily, norfloxacin 400 mg 2 × daily or ofloxacin 200 mg 2 × daily) or second-line drugs.
2. Second-line drugs: amoxicillin/Clavulanate orally 625 mg 2 × daily for 3–7 days, Cefaclor 250 mg 3 × daily for 3–7 days, amoxicillin 500 mg 3 × day for 7–10 days (not used for empiric therapy).
If concomitant acute pyelonephritis is suspected (e.g. dysuric symptoms persisting for > 5-7 days, lumbar pain for no other obvious cause, unconfirmed fever, but subjective sensation of fever) cotrimoxazole or fluoroquinolone is used.
3. Post-treatment follow-up: Post-treatment follow-up studies are not recommended in asymptomatic patients.
2) Recurrent cystitis in women. Recurrent bladder inflammation occurs in 10–20% of women without risk factors for complicated UTI. The etiological factors are the same as in sporadic uncomplicated bladder inflammation. Re-infection is much more common than relapse. Some women have a clear connection between intercourse and consecutive episodes of UTI. In general, imaging and other studies are not recommended unless you suspect risk factors for complicated UTI and urine culture detects a microorganism typical of uncomplicated UTI (E. coli, S. saprophyticus). The detection of a rare uropathogen (e.g. Proteus sp.) leads to suspicion of a complicated UTI.
Treatment
1. Use drugs as for uncomplicated bladder inflammation (see number 1 of the list).
2. In some cases, repeated UTI is caused by recurrent infection; most often, when the previous inflammation of the bladder was accompanied by asymptomatic pyelonephritis, which was not cured after using short-term antibiotic therapy. In case of recurrence of UTI, urine culture should be done and antibiotic therapy should be continued for 2–6 weeks.

3) Acute uncomplicated pyelonephritis (kidney infection) in women. Uncomplicated AP is the result of an rising infection from the lower urinary tract. Infection and inflammation concern the calyx-pelvis system and the adjacent parenchyma of the renal medulla. The clinical picture is different: from symptoms of cystitis (subclinical AP occurs in 30-50% of cases of uncomplicated cystitis) to urosepsis. Typically, varying degrees of lumbar pain, feeling unwell, chills, and fever occur within<24 hours; dysuric disorders and nausea and vomiting may be present. Objective research determines a positive symptom of tapping in the lower back, usually unilateral, and sometimes sensitivity in the hypogastrium due to inflammation of the bladder, which preceded the AP and is still ongoing.
In each case, before starting treatment, a physical examination and urine culture should be carried out, and in hospitalized patients also a blood culture. Leukocyturia is almost always present, urine culture is positive in 90% of cases (bacteriuria usually ≥105 CFU/ml). Imaging studies are indicated when there is doubt about the diagnosis, fever persisting for s> 48 hours, worsening of the clinical condition during treatment, the need for hospitalization, with a repeated episode of AP.
Treatment
Treatment should be based on urine culture and last 10-14 days. Empiric therapy should be used pending results.
1. Patients with mild symptoms, in good general condition and adhering to medical recommendations: can be treated on an outpatient basis.
1) First-line drugs - fluoroquinolones orally for 7-10 days (e.g. ciprofloxacin 500 mg 2 × a day or Levofloxacin 500 mg 1 × a day);
2) Alternative drugs (if the first-line drug cannot be used) orally for 10-14 days: Cefpodoxime 200 mg × daily, Ceftibuten 400 mg 1 × daily, Cotrimoxazole 960 mg 2 × daily, amoxicillin with clavulanic acid 1,0 g 2 × per day.
If the resistance of community-acquired E. coli strains to fluoroquinolones is ≥10% in the region and if alternative drugs are used, treatment should be started with a single dose of a long-acting parenteral antibiotic (e.g. Ceftriaxone 1.0 g or daily dose of aminoglycoside).
2. Patients requiring inpatient treatment: hospitalization is indicated in case of persistent nausea and vomiting, no improvement or exacerbation of symptoms, despite outpatient treatment, doubt about the diagnosis, pregnancy. The drugs are usually given intravenously (IV), initially empirically, with one of the following antibiotics:
1) Fluoroquinolone - usually 200-400 mg IV every 12 hours (not used during pregnancy);
2) Aminoglycoside - gentamicin 5-7 mg/kg IV 1 × a day (or 1 mg/kg IV every 8 hours) as monotherapy or with Ampicillin (1.0 g IV every 6 hours);
3) III generation cephalosporin, for example. Ceftriaxone 1–2 g IV 1 × daily.
Treatment is modified after urine and blood cultures are obtained. The disappearance of fever and clinical improvement (usually within 72 hours) are the conditions for switching to oral treatment with an antibiotic selected based on the results of microbiological studies (not necessarily the same one that was injected intravenously). In asymptomatic patients, follow-up studies are usually not required after treatment.
4) Complicated UTIs. The most common factors due to which UTI should be considered as complicated are male gender, diabetes mellitus, pregnancy, nephrolithiasis (kidney stones), an obstruction in the outflow of urine.
The clinical picture is different: from mild cystitis to urosepsis (urinary tract sepsis, a potentially life-threatening condition caused by the body's response to an infection). In each case of diagnosis or suspicion of a complicated UTI, a general analysis and urine culture, as well as biochemical blood tests, should be performed to assess kidney function. In cases of moderately severe to severe disease in hospitalized patients, blood cultures should be performed. In each case, an ultrasound scan should be done, and in some patients also an overview x-ray of the abdominal cavity, in order to exclude urolithiasis and obstructions in the urinary tract with difficulty in the outflow of urine. Indications for performing other imaging studies: suspected kidney and perirenal complications of UTI, other concomitant abnormalities in the abdominal cavity or pelvis, and diagnosed changes in the urinary tract.
Treatment
1. Depending on the severity of symptoms and concomitant diseases, treatment is carried out on an outpatient basis or in a hospital. Indications for hospitalization: urinary tract anomalies, decreased immunity, renal failure, other concomitant severe diseases, other - as in uncomplicated AP.
2. Urological intervention: in many cases it is essential; the goal is to remove the anomalies in the urinary tract, while antibiotic therapy is an adjunct.
3. Empirical treatment of complicated UTI: according to the same principles as in uncomplicated AP. If empiric treatment is ineffective and microbiological results are not available, it is recommended to use a broad-spectrum antibiotic active against Pseudomonas spp. (e.g. ceftazidime, cefepime, piperacillin with tazobactam, carbapenem) and an aminoglycoside (preferably amikacin) should be considered if not already used. Oral therapy and duration of treatment are as in uncomplicated AP.
4. Outpatient treatment: The first line drugs are fluoroquinolones.
5. Treatment in young men without additional risk factors for complicated UTI: should last 7 days in case of symptoms of inflammatory process in the bladder, and 14 days if there are signs of AP.
6. Control urine culture: should be repeated 1–2 weeks after completion of therapy.
5) Asymptomatic bacteriuria (symptomless UTI)
Diagnostic

The diagnosis of UTI is determined on the basis of subjective and objective manifestations and the results of additional research methods.
Additional research methods
1. General urine analysis: leukocyturia, leukocyte casts (evidence of kidney inflammation), hematuria (blood in urine).
2. Urine culture:
1) You can assume that uncomplicated cystitis in an out-of-hospital woman is caused by E. coli or S. saprophyticus and proceed without urine culture;
2) Bacteriological examination of urine should be done in all incidences of UTI and in women with signs of bladder inflammation, if standard empirical treatment was ineffective, suspect a complicated UTI, or if the present UTI occurred within one month from the preceding episode;
3) Test strips are intended only for preliminary research in the diagnosis of UTI based on the detection of nitrites in urine, which are produced from nitrates by Escherichia coli (Enterobacteriaceae). Their sensitivity allows the detection of bacteria in an amount> 105 CFU/ml. For this reason, and because they do not detect bacteria that do not produce nitrite, test strips cannot replace urine cultures when indicated.
4) In ≈30% of cases of dysuria (painful or difficult urination) caused by infection, the result of standard bacteriological examination (culture) of urine is negative (so-called non-bacterial inflammation of the bladder or urethra see below).
3. Blood tests: leukocytosis, increased ESR, increased concentration of CRP.
4. Blood culture: a positive result is possible in severe forms of UTI.
5. Imaging studies: should be appointed in complicated UTI, and uncomplicated AP in women, if manifestations of infection are maintained or aggravate despite standard therapy. Ultrasound of the urinary system - allows detecting anomalies of the urinary system (e.g. kidney stones, urinary retention, cysts, tumors) and complications of UTI (kidney and perirenal abscess). Urography - is appointed mainly in case of suspicion of anomalies of the calyx-pelvic system or ureters. CT with the introduction of a contrast agent - has the highest sensitivity for identifying perirenal abscesses, allows visualizing focal bacterial inflammation of the kidneys. DMSA kidney scintigraphy is a very sensitive test for detecting OP.
Diagnostic criteria
UTI is diagnosed based on clinical symptoms; one should always try to confirm them by doing a urine culture (besides uncomplicated cystitis in women, which is diagnosed based on clinical symptoms only). Presence of large number of bacteria confirms an UTI in a symptomatic person.
Differential diagnosis
Other diseases that can cause urinary disorders and pain complaints localized in the pelvic region (diseases of the genitals, prostate), kidney colic, inflammation of the abdominal organs.
Prevention

Recurrent UTI is most often uncomplicated cystitis, much less often uncomplicated AP. The following are methods of prophylaxis recurrent uncomplicated UTI. Relapses of uncomplicated UTI are a separate clinical problem associated with urinary tract abnormalities, impaired immunity, or resistance of uropathogenic microorganisms to antimicrobial drugs.
Non-pharmacological methods
All women with recurrent UTI should be advised:
1. Increase the amount of fluid they drink (including an extra glass of fluid before intercourse).
2. Urination immediately after the onset of the urge or regularly every couple of hours, and right before bedtime and after intercourse.
3. Avoid using intimate deodorants, cervical caps and vaginal spermicides.
4. Avoid bubble baths and adding chemicals to the bath.
Pharmacological methods
1. Vaginal use of preparations with Lactobacillus.
2.Vaginal application of estrogen cream (in postmenopausal women).
3. Prophylactic antibacterial treatment (options):
1) Treatment, when clinical symptoms occur, undertaken by a woman herself according to the rules, as in uncomplicated inflammation of the bladder (see below). This strategy is recommended when the number of episodes of UTI per year is ≤3. Advise the patient to contact her doctor if symptoms persist within 48 hours or are unusual.
2) Prevention after intercourse - a single dose after intercourse. Medicines and doses, as in the case of continuous prophylaxis, either ciprofloxacin 250 mg or cephalexin 250 mg. This strategy is advised when the number of UTI episodes during the year is > 3 and there is a clear temporal association with intercourse.
3) Continuous prophylaxis - every day before bedtime or 3 times a week, orally cotrimoxazole 240 mg, trimethoprim 100 mg or norfloxacin 200 mg; initially within 6 months. If after this period, recurrence of UTI still occurs, continue prophylaxis for ≥2 years.
Post by: Jacob Hansen, General healthcare practitioner, National health centre, Stavanger, Norway
(Updated at Apr 13 / 2024)
Macrobid articles:
Some of the trademarks used in this Web Site appear for identification purposes only.
All orders are reviewed by a licensed physician and pharmacist before being dispensed and shipped.
The statements contained herein are not intended to diagnose, treat, cure or prevent disease. The statements are for informational purposes only and is it not meant to replace the services or recommendations of a physician or qualified health care practitioner. If you have questions about the drugs you are taking, check with your doctor, nurse, or pharmacist.