What is angina and how is it treated?


Angina pectoris is a specific pain syndrome characteristic of myocardial ischemia. Stable and unstable angina pectoris, as well as exertional and rest angina pectoris, are distinguished.
Stable angina pectoris is one that proceeds unchanged. We can say that this is a "habitual" symptomatology for a person. However, this situation cannot be considered the norm: serious treatment is required, often surgical.
Unstable angina pectoris is either a new-onset angina pectoris, or one when the nature of the pain syndrome and sensations differs significantly from the usual state. This is an extremely dangerous condition, fraught with a high risk of developing a heart attack, and requiring an immediate call for an ambulance.
Exertional angina pectoris is one of the manifestations of atherosclerosis and coronary heart disease, which is manifested by severe chest pain during physical activity and stress. However, chest pain is not always a manifestation of angina pectoris.
It is important to note symptoms such as:
- Constricting, pressing or burning character of the attack;
- Recoil under the left shoulder blade or in the arm, neck, lower jaw;
- Lack of oxygen and dizziness;
- Obvious interruptions in the work of the heart: fluctuations in heart rate and blood pressure.
Most often, pain with angina pectoris is manifested during walking, climbing stairs, physical effort, stress. The attack lasts 1 to 15-20 minutes and is relieved by taking nitroglycerin. Symptoms can appear all at once or separately.
Rest angina pectoris, in contrast to the previous type, is characterized by a sudden and prolonged attack, which is activated without external provoking factors, sometimes during sleep. In this case, you can add to the main symptoms: an uncontrolled panic attack, a pronounced feeling of suffocation, a violation of the autonomic functions of the body. We will write more about this type of angina pectoris in the following articles.
In addition to extremely unpleasant symptoms, such manifestations indicate a high risk of myocardial infarction, as well as the development of heart failure.
Cardiovascular diseases claim half of human lives - exactly the same as all other causes combined.
Causes of angina
The cause of angina pectoris is the partial overlap of the lumen of the arteries by atherosclerotic plaques, as a result of which there is a pronounced oxygen deprivation of the heart cells, which causes pain. An additional role is played by vasospasm, which can be provoked, for example, by nervous overstrain or exiting outside in low temperature.
It is the presence of atherosclerotic plaques that is the leading factor in the development of angina pectoris. The development of coronary heart disease is a complex and multicomponent process that is provoked and accelerated due to risk factors:
- Arterial hypertension,
- Smoking, obesity,
- Violation of cholesterol metabolism,
- Diabetes,
- Low physical activity and poor nutrition.
In the case of atherosclerosis, angina pectoris begins to manifest itself when an atherosclerotic plaque fills the artery by more than 50% - it prevents the normal passage of blood through the heart and, accordingly, the saturation of the heart muscle with oxygen. This leads to the development of an imbalance in the work of the heart.
With physical and psycho-emotional stress, the situation is aggravated. The heart begins to work more actively - it contracts more often and stronger. In this state, he needs more oxygen and nutrients. However, due to vasoconstriction, this need is not satisfied, which leads to oxygen starvation and, as a result, pain.
We feel pain thanks to the instinct for self-preservation. It is a kind of alarm. Therefore, any painful attack is a rational reason to see a doctor.
Risk factors and their control
Angina pectoris and the diseases due to which it manifests itself require not only the fastest possible treatment, but also the control of risk factors. These include:
- Hyperlipidemia - an imbalance in cholesterol metabolism. It is characterized by an increased concentration of low density lipoproteins and fatty acids - triglycerides. And also a decrease in the level of high density lipoproteins - "good" cholesterol.
It is observed in most patients with angina pectoris. Lowering cholesterol levels in the body can help reduce seizures.
- Obesity - characterized by a body mass index of more than 26 and, often, arises from constant inappropriate nutrition: consumption of high-calorie foods high in animal fats, cholesterol and "fast" carbohydrates such as sugar and starchy foods. And, on the contrary, a lack of vegetables, fruits, whole grains, legumes, herbs in the diet. In addition, a large body weight increases the burden on the heart, the risk of an attack increases. To control this factor, it is necessary to adhere to the principles of rational or healthy nutrition: limit the intake of cholesterol, animal fats, processed foods and salt. Increase your intake of vegetables, fruits, and other whole plant foods containing fiber, natural antioxidants, polyphenols, and flavonoids. Overweight is usually just the tip of the iceberg. This is a manifestation of serious imbalances in the body.
- Physical inactivity - inadequate physical activity, combined with poor diet, contributes to the risk of obesity and the accumulation of cholesterol. Together, these factors contribute to the development and frequent manifestation of angina pectoris.
- Arterial hypertension - is a frequent companion of coronary heart disease, which, in itself, implies oxygen deficiency of the myocardium. With an increase in blood pressure, the myocardium is stressed, which causes an even greater demand for oxygen in the heart. This provokes an attack of angina pectoris. Controlling blood pressure will help keep the heart and blood vessels relatively calm - reducing the frequency and intensity of attacks.
- Anemia is not a risk factor, but a condition that aggravates the course and makes it difficult to control ischemic heart disease. It is characterized by a reduced level of hemoglobin and a general weakening of the body, hence the impossibility of adequately supplying the heart with oxygen. Controlling the normal level of hemoglobin in the blood helps to alleviate the course of the disease: for women, the norm is 120-150 g/l, for men - 135-165 g/l.
- Tobacco addiction - smoking increases several risk factors at once: it causes oxygen starvation, increases blood pressure and causes spasms of the arteries. The habit is harmful to a healthy body, and in the presence of atherosclerosis leads to early manifestations of angina pectoris and significantly increases the risk of acute myocardial infarction.
- Diabetes mellitus type 2. This disease seriously worsens the course and prognosis of ischemic heart disease. We have a separate article to this condition, but for now we draw attention to it as a serious risk factor for angina.
The combination of 2 or more items from the list, even mild ones, increases oxygen deprivation of the heart, and, accordingly, the risk of developing and the severity of angina symptoms. The presence of risk factors should be taken into account when determining treatment tactics and secondary prevention of angina pectoris.
Diagnostics of angina
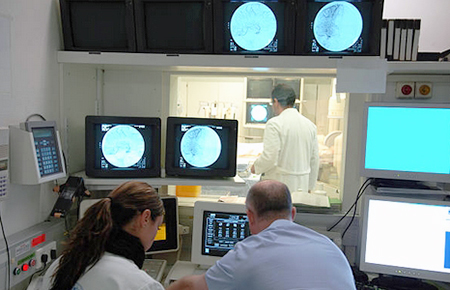
To diagnose angina pectoris, as well as to exclude other possible diseases, they analyze complaints and the nature of pain, conduct a laboratory blood test and a functional examination of the heart, analyze the patient's physical condition.
It is also important to determine the severity of the process. For this, if an acute coronary syndrome is diagnosed, a study of the vascular bed of the heart is performed - coronary angiography. Based on the results, the question of surgery or intravascular intervention is decided.
Laboratory blood tests help determine the level of:
- Total cholesterol and lipid fractions,
- High and low density lipoproteins,
- Triglycerides,
- Creatine kinase,
- Glucose,
- Markers of systemic inflammation (CRP),
- Indicators of the coagulation system - coagulograms,
- Electrolytes,
- Troponin - in acute situations.
The study pays special attention to the presence of cardiac troponins I and T - markers that report myocardial damage. Their presence confirms that the patient is suffering a microinfarction or acute myocardial infarction.
Functional research methods allow to determine state of the heart:
- ECG - examination at the peak of an attack of angina pectoris detects conduction and rhythm disturbances. Signs of myocardial oxygen deprivation may also be detected.
- Daily ECG monitoring - records the level of oxygen deprivation during an attack of angina pectoris, heart rate, arrhythmia. The indicators help determine the specific diagnosis and stage of the disease.
- EchoCG - detects local ischemic changes and violations of myocardial contractility.
- Bicycle ergometry or treadmill - determines the maximum possible physical activity for the patient without the threat of ischemia. The load is set using an exercise bike or treadmill, and the results are recorded by an ECG machine.
- Stress echocardiography (Stress ECHO) - the study of myocardial contractility by ultrasound, in conditions of dosed physical activity. An ECG is recorded at the same time. Allows making the primary diagnosis of ischemic heart disease, clarifying the indications for surgical treatment.
For a detailed study of the vascular bed of the heart, the following are used:
- Coronary angiography - an X-ray method in which a contrast agent is injected into the artery of the heart using a special catheter.
- Multispiral computed tomography - a type of computed tomography in which x-ray "slices" of the heart and blood vessels are obtained at high speed. More than 100 of these "slices" can be made between the contractions of the heart chambers.
These studies allow doctors to obtain information about the state of the vascular bed of the heart: which arteries are passable, which are fully or partially blocked, in what place. Based on the information received, the doctor decides whether the patient has coronary artery disease, the need for surgery and the timing of treatment.
Stages/classification of angina severity
Treatment of angina
Angina pectoris is an accompanying factor of coronary heart disease, therefore, the main fight must be waged with it. Treatment of angina pectoris is aimed at stopping and preventing attacks and complications.
The first priority when an attack occurs is taking nitroglycerin. It helps relieve pain. If the attack persists, nitroglycerin can be reused.
Drug therapy involves the prescribing of anti-ischemic drugs by the attending physician to help the heart cope with low oxygen levels. The first-line drugs are Beta-blockers and calcium channel antagonists (Plendil). Anti-sclerotic drugs, antioxidants and antiplatelet agents are also prescribed.
Based on the diagnosis, a decision is made on additional treatment for cardiac conduction and rhythm disorders. For angina pectoris, surgery is often prescribed: balloon angioplasty, stenting, coronary artery bypass grafting.
Forecast and prevention of angina

Angina pectoris is a dangerous heart disease. Lack of attention to the disease leads to the development of myocardial infarction and increases the risk of death. At the same time, a competently and timely formed plan of treatment and secondary prevention of angina pectoris and its causes helps to control the state of the body and prevent disastrous consequences - to keep life joyful and fulfilling.
Prevention of angina attacks involves the elimination of risk factors:
- Reduction of excess weight;
- Blood pressure control;
- Diabetes control;
- Maintaining a healthy lifestyle: smoking cessation, good nutrition, physical activity;
- Learn coping with stress (meditation, yoga, hobbies, etc.).
Post by: Jacob Hansen, General healthcare practitioner, National health centre, Stavanger, Norway
(Updated at Apr 14 / 2024)
Plendil articles:
Some of the trademarks used in this Web Site appear for identification purposes only.
All orders are reviewed by a licensed physician and pharmacist before being dispensed and shipped.
The statements contained herein are not intended to diagnose, treat, cure or prevent disease. The statements are for informational purposes only and is it not meant to replace the services or recommendations of a physician or qualified health care practitioner. If you have questions about the drugs you are taking, check with your doctor, nurse, or pharmacist.