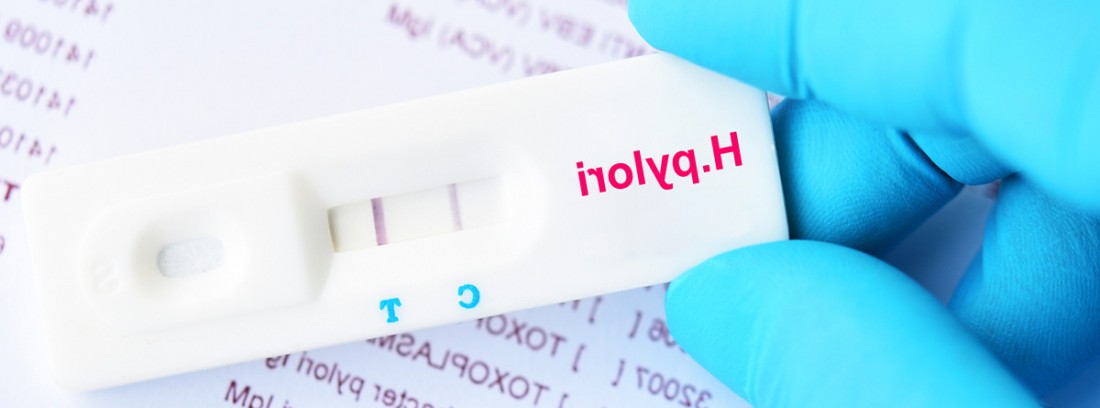
Helicobacter pylori or breath test
It is the most prevalent infection in the world. Various techniques are available that make it possible to diagnose the presence of Helicobacter pylori and to assess its eradication after appropriate treatment. The non-invasive diagnostic test of choice is the breath test.
What is Helicobacter pylori?
Helicobacter pyloriit's a bacteria discovered in 1983 by Robin Warren and Barry Marshall, who linked it to the appearance of and, for whose discovery, they were awarded the Nobel Prize in Medicine in 1995.
This bacillus chronically infects the gastric mucosa, it is the most prevalent infection on the planet and affects 50% of the population. The route of transmission is not clear and it mainly happens during childhood, among children, by the fecal-oral or oral-oral route. Most infected people have no symptoms, but Helicobacter pylori infection can cause some different, such as or diseases such as peptic ulcer (affects 10-20% of infected patients) and the gastric cancer (affects less than 1% of infected patients).
In infected people, Helicobacter lives in the mucous layer of the stomach where, thanks to specific enzymes called ureases, produces ammonia and partially neutralizes the natural acidic pH of the stomach in order to grow and survive.
Symptoms
It is important to see our reference doctor when these symptoms appear:
- Recurring burning sensation, pain, or heartburn in the upper abdomen, under the breastbone.
- Gastralgia or chronic stomach pain.
- Abdominal distension.
- Early satiety
- Lack of appetite.
- nausea and vomiting
- Black stools
- Anemia and tiredness
How is it diagnosed?
Various techniques are available that make it possible to diagnose the presence of Helicobacter pylori and to assess its eradication after appropriate treatment.
Diagnostic methods for Helicobacter pylori infection are classified as "invasive" and "non-invasive."
The non-invasive tests do not require endoscopy and would be:
- 13C-labeled urea breath test
- Determination of antigen in feces.
- Serological blood test.
Invasive methods are based on direct bacterial detection techniques that require and biopsy. Not all samples can contain the bacteria, so it is not always very sensitive to diagnose but to detect more serious diseases such as.
Current protocols recommend checking the cure of the infection after treatment in all cases with the breath test or the monoclonal antigen in stool.
The diagnostic indications are:
- Recurrent abdominal pain and dyspepsia.
- Peptic ulcer.
- Patients with MALT lymphoma or stomach cancer.
- First-degree relatives of patients with gastric cancer.
- Gastric mucosa atrophy.
- Iron deficiency anemia without apparent cause.
- Idiopathic thrombocytopenic purpura.
- Vitamin B12 deficiency not explained by other causes.
The breath test
The non-invasive test of choice is the urea breath test marked with 13C. It is based on the urease activity of Helicobacter pylori to transform urea. To perform the test, a urea tablet labeled with a non-radioactive isotope is administered: the carbon 13 (13C). In the presence of Helicobacter pylori, the marked urea is degraded into carbon dioxide (CO2) and ammonia (NH3). The marked CO2 is absorbed, passes into the blood and is eliminated as exhaled air through the lungs. Therefore, 13C can be easily detected in an expired air sample. This test is much more reliable and sensitive if a drink of citric acid. This avoids the appearance of false negatives.
Using specially designed devices, the CO2 marked in the exhaled air can be detected and the presence of the bacteria confirmed.
Helicobacter pylori infection can be treated by using a combination of antibiotics. This eliminates the infection and heals the ulcer in about 80% of cases. If the bacteria cannot be killed, the ulcer reappears after a short time in most people.
How is the breath test performed
This test is done on an outpatient basis. Admission is not required, but the presence of qualified health personnel is required to carry it out.
For the breath test they must stop taking inhibitors proton pump (omeprazole), at least two weeks before of the evaluation. Yes, antacids can be taken. It is also recommended to avoid any antibiotic treatment and / or bismuth salts for at least four weeks before the test.
It is completely painless and does not cause discomfort.
While the test is running, the patient will be seated. Two samples are taken: the one we call "baseline" and the "diagnostic" one. First, a basal determination is carried out, 10 minutes after taking the citric acid, in which you must blow continuously into the sample container, which will be closed immediately. Subsequently, the tablet containing the labeled urea is supplied. After 30 minutes, the second respiratory sample will be collected.
The samples can be analyzed immediately or be sent to the reference laboratory for analysis. After the test, the patient can return home.
Breath test precautions
This is a safe test. It uses a natural, non-radioactive isotope of carbon, so it can be repeated, even in pregnant women. In less than 0.1% of cases, abdominal distention, diarrhea, and epigastric discomfort may occur.
- If the patient is allergic To the active principle (urea) or to any of the components of the test, this test cannot be performed. In addition, patients with phenylketonuria cannot perform this test.
- In case dand children under the age of five It would not be the test of choice to detect Helicobacter pylori, since its capacity for collaboration may be low and we would use the antigen in feces.
- In gastrectomized patients (for those whose stomach has been partially removed) or who suffer from atrophic gastritis, the breath test may not be the most indicated screening test.
If during the test the patient vomits, it is necessary to repeat it, at least, the next day on an empty stomach.
- Helicobacter pylori infection affects approximately 50% of the population and can cause chronic gastritis, peptic ulcer, and gastric cancer.
- The noninvasive diagnostic test of choice is the 13C-labeled urea breath test.
- Using specially designed devices, the CO2 marked in the exhaled air can be detected and the presence of the bacteria confirmed.
Pediatrician Teladoc Health Collaborating Physician
(Updated at Apr 13 / 2024)