Placenta accreta
The incidence of placenta accreta has increased in recent years since several of its risk factors have also increased (previous uterine surgeries, previous deliveries, being over 35 years old ...).
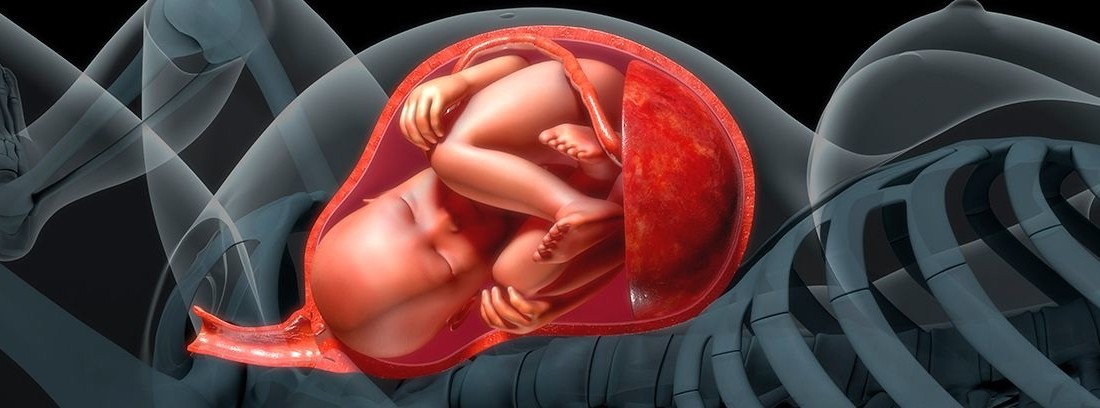
A normal delivery has three phases:
- Dilatation: phase in which the cervix is erased and dilated with contractions, until the neck is fully dilated, this is 10 cm.
- Expulsive: phase in which the fetal head descends into the pelvis until the fetus has completely emerged.
- Delivery: the fetus has already come out and the placenta and membranes are shed and expelled.
Patients with a placenta accreta have a pathological phase of labor since the placenta cannot be delivered in the normal way. Part or all of the placenta remains attached to the wall of the uterus and causes excessive bleeding.
Placenta accreta symptoms
The accreta placenta generally it does not give any symptoms until the delivery period of labor, although in some occasions by ultrasound there may be some suspicion. Sometimes an MRI can be performed for a better visualization of the insertion of the placenta if doubts remain.
Risk factor's
The risk factors are:
- Previous uterine surgery: previous cesarean section, myomectomy….
- : the placenta is in front of the cervix and prevents the passage of the fetal head.
- Mother's age: over 35 years of age, the accreta placenta is more common.
- Previous deliveries: the risk of accreta placenta increases proportionally to the number of previous deliveries.
Complications of the placenta accreta
The placenta accreta has traditionally been a maternal mortality risk factorHowever, in recent decades, mortality from placenta accreta has decreased from 9.5% to less than 1%.
The most severe grade of placenta accreta is placenta percreta in which the placental tissue completely crosses the wall of the uterus and it can invade neighboring organs such as the urinary bladder. In these cases, in addition to a risk of mortality over 7%.
Excessive bleeding from a poorly inserted placenta often leads to need for blood transfusion. If the placenta is percrete, it can force a surgery is that the affected organs must be reconstructed, such as the urinary bladder, with the consequent possible involvement of these organs in a definitive way.
The importance of early diagnosis
The prognosis of placenta accreta depends on several factors, but a very important one is the time of diagnosis. The patient with a suspicion of placenta accreta during pregnancy and surgery may be scheduled With a multidisciplinary team and with blood in reserve in case it is necessary, that the patient who has a normal delivery and at the moment of waiting for the delivery a significant hemorrhage occurs and an urgent surgery has to be carried out.
But most of the time the diagnosis is made at the moment of delivery and therefore is not programmed. The insurances have a wide medical staff in gynecology and obstetrics so your pregnancy will always be in the best hands.
How to proceed then ...
The most common is having to perform a urgent hysterectomy, that is, remove the womb to avoid massive bleeding. In this case, the ovaries would be preserved so that the patient would not be menopausal but would not have her period as she did not have a womb nor could she bear more children.
Sometimes it is possible to remove whole placenta with a uterine curettage With a large curette, which is an instrument shaped like an empty spoon in the center and around the edges, scratch the surface against which it is scratched.
But the risk of this treatment is that the abrasion on the inner face of the matrix If the bleeding occurs even more abundantly or if a lesion occurs that crosses the entire thickness of the wall of the uterus, one has to be very cautious with a curettage in an accreta placenta.
Finally, and in very few cases, conservative treatment is achieved by allowing the placenta to dissolve over time, especially in the cases of focal accreta, that is, of a part and not of the whole of the placenta.
The risk of conservative treatment is the possibility of heavy vaginal bleeding, risk of infection of the remaining tissue and of the womb, risk of a tissue embolism or by a blood clot and risk of having to perform a hysterectomy later due to failure in the absorption of the remaining placental tissue.
In cases of conservative treatment, a antibiotic regimen of at least 10-14 days and carry out weekly controls.
- In childbirth, the placenta cannot be delivered in the normal way. Part or all of the placenta remains attached to the wall of the uterus and causes excessive bleeding.
- The incidence of placenta accreta has increased in recent years since several of its risk factors have also increased (previous uterine surgeries, previous deliveries, being over 35 years old ...)
- The prognosis of placenta accreta depends on several factors, but a very important one is the time of diagnosis.
Specialist in gynecology and obstetrics
(Updated at Apr 14 / 2024)