What causes female infertility and how to treat it?

Infertility is an inability of an individual of childbearing age to have children due to the impairment of the fertilization or implantation of the fertilized egg. Infertility in a woman should be established only after her partner’s infertility is excluded and after the positive tests confirming the compatibility of the sperm and mucus of the cervix.
Short information about female infertility
Different types of female infertility are distinguished
– Primary and secondary (based on the presence or absence of previous pregnancies);
- Relative (the probability of pregnancy is not excluded);
- Absolute (pregnancy is impossible due to the absence of the uterus, ovaries, fallopian tubes due to malformations or surgical interventions).
According to the WHO classification, there are four main groups of causes of infertility in women:
- Ovulation disorders - 40%
- Tubal factors (pathology of the fallopian tubes) - 30%
- Various gynecological diseases not accompanied by impaired ovulation and the function of the fallopian tubes - 25%
- So-called unexplained infertility - (5%), in which there are no visible causes of reproductive dysfunction. The frequency of this type is constantly decreasing when using modern research methods (for example, it turns out that in some women it is caused by immunological reasons - immunological infertility).
WHO recommends the following scheme for examining women with infertility:

- Functional diagnostics tests during two menstrual cycles;
- Blood tests for prolactin, testosterone, dehydroepiandrosterone (with hyperandrogenism, the study is carried out before and after taking dexamethasone);
- Metrosalpingography on the 6-8th day of the menstrual cycle;
- Ultrasound biometry of follicles on the 8-14th days of the menstrual cycle (or after taking ovulation stimulants);
-Postcoital tests on the 12-14th day of the menstrual cycle;
- Laparoscopy on the 18-20th day of the menstrual cycle;
- Determination of the content of progesterone in the blood and (or) pregnandiol in the urine on the 19-24th day of the menstrual cycle;
- Biopsy of the endometrium 2-3 days before the onset of menstruation.
Infertility due to ovulation disorders (endocrine infertility)
Infertility can be caused by:
- Lack of ovulation (anovulation),
- Insufficiency of the luteal phase,
- Unovulated follicle luteinization syndrome.
Anovulation

Anovulation (absence of ovulation) is a symptom of many endocrine diseases (polycystic ovary syndrome, congenital dysfunction of the adrenal cortex, Cushing's disease, galactorrhea-amenorrhea syndrome, postpartum neuro-endocrine syndrome, hypo- and hyperthyroidism), nervous and various genes, obesity.
Chronic anovulation can be a consequence of dysfunction of the hypothalamic-pituitary system (disturbance of the rhythm of release of luliberin and gonadotropins), which developed after neuroinfection, intoxication, psychoemotional stress, trauma, childbirth, etc.
Clinical manifestations of chronic anovulation, in addition to infertility, are menstrual bleeding disorders - dysfunctional uterine rheumatism, amenorrhea.
The absence of ovulation is confirmed by functional diagnostics tests: monophasic basal temperature, monotonic karyopycnotic index, cervical mucus tension 2-6 cm.
For diagnostic purposes, laparoscopy is used. It allows assessing the state of the ovaries - to detect the absence of ovulatory stigma (places of rupture of the follicle) and yellow bodies, signs of polycystic ovaries, to identify non-endocrine causes of infertility - adhesions in the small pelvis, obstruction of the fallopian tubes, external endometriosis, etc.
Luteal phase failure
Insufficiency of the luteal phase, or hypofunction of the corpus luteum is accompanied by a decrease in the synthesis of progesterone and can lead to infertility due to a decrease in the peristaltic activity of the fallopian tubes in the second phase of the menstrual cycle, the inadequate secretory transformation of the endometrium and impaired implantation of fertilization of the egg.
As a physiological phenomenon, NLF can be observed in the first menstrual cycles after childbirth, abortion or withdrawal of hormonal contraceptives, in pre-menopause.
Luteal phase insufficiency can be caused by:
- Hyperandrogenism of the adrenal and ovarian origin (congenital dysfunction of the adrenal cortex, polycystic ovaries, etc.),
- Functional hyperprolactinemia (galactorrhea syndrome - amenorrhea),
- Chronic inflammatory diseases of the uterine appendages, hypothyroidism.
In addition to infertility associated with luteal phase insufficiency, scanty spotting is often noted a week before the start of the next menstruation.
The diagnosis is made on the basis of a shortening of the hyperthermic phase of the menstrual cycle to 8-4 days when the difference in basal temperature in the first and second phases of the cycle is less than 0.4 ; the content of pregnandiol in urine less than 3 mg/day and progesterone in the blood less than 15 nmol/l on the 4th day of an increase in basal temperature; defective phase of secretion in the endometrium, biopsied 2-3 days before the onset of menstruation.
Luteinization syndrome of non-ovulated folliclela
The syndrome of non-ovulated follicle luteinization (LNF) has not been adequately studied.
It is assumed that stress, hyperprolactinemia, and oophoritis play a role in its occurrence.
Diagnosis of SLNF is difficult, since the content of pregnandiol in the urine, progesterone in the blood, basal temperature, and endometrial state in the second phase of the menstrual cycle are the same as in the ovulatory menstrual cycle. With ultrasound biometry in the second phase of the menstrual cycle, a slow gradual decrease in the follicle is noted. On the 14-15th day of the menstrual cycle, laparoscopy reveals a hemorrhagic corpus luteum without ovulatory stigma.
Endocrine infertility treatment
Treatment of endocrine infertility is carried out in the absence of somatic diseases in a woman and if her age does not exceed 35 years.

- In case of infertility due to anovulation, treatment of the diseases that caused anovulation is necessary. If there is no effect from the treatment of the underlying pathology, ovulation is stimulated. The effectiveness of ovulation stimulation is determined by dynamic monitoring of the follicle size (ultrasound biometry). A follicle diameter of 20 mm or more indicates that the preovulatory stage has been reached, the subsequent disappearance of the follicle indicates that ovulation has taken place.
- In case of infertility associated with luteal phase insufficiency, pathogenetic treatment of diseases that cause dysfunction of the ovaries is carried out. In addition, progesterone replacement therapy is prescribed in the second phase of the menstrual cycle. Duphaston is frequently used as a first-line treatment. The duration of treatment is determined individually (usually, it is performed for at least 3-4 menstrual cycles).
- In case of infertility due to the syndrome of luteinization of the non-ovulated follicle, ovulation is stimulated.
Forecast
The prognosis for the restoration of fertility with timely rational therapy of endocrine infertility is generally favorable.
With the onset of pregnancy, careful observation from the early stages and hospitalization are necessary at the slightest sign of the threat of termination of pregnancy. In childbirth, weakness and discoordination of labor often develop.
Infertility due to tubal factors
The tubal factors of infertility include functional and organic pathology of the fallopian tubes.
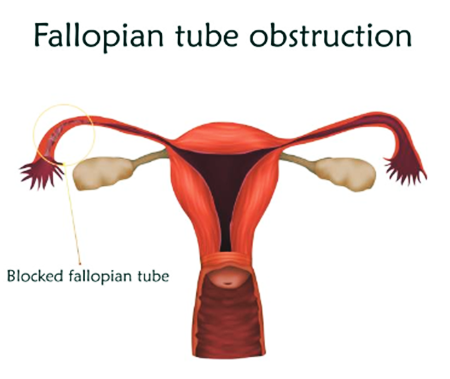
The functional pathology of the fallopian tubes is characterized by a violation of their contractile activity (hypertonicity, hypotension, discoordination) due to inflammatory processes in the small pelvis (including in the uterine appendages), violations of the hormonal function of the ovaries, and changes in the ratio of estrogens and progesterone in the body, hyper- or hypoprostaglandinemia , hyperandrogenism.
Organic pathology of the fallopian tubes, leading to infertility, includes obstruction, adhesions, torsion, condition after surgery on the fallopian tubes. It can be a consequence of pelvic inflammatory disease, pelvioperitonitis, endometriosis of the fallopian tubes, as well as complications after childbirth, abortion, operations on the abdominal organs (for example, after surgery for phlegmonous appendicitis, tubal infertility develops 5 times more often than in women, who have not undergone appendectomy).
To diagnose tubal infertility, metrosalpingography is used with the use of water-soluble X-ray contrast agents on the 6-8th day of the menstrual cycle (in the second phase, a mucous plug or folds of the secretory endometrium in the mouth of the fallopian tubes can prevent the penetration of contrast agent into the fallopian tubes); laparoscopy with simultaneous chromohydrotubation with indigo carmine or methylene blue solutions, which allows you to establish the site of impaired patency of the fallopian tubes and identify other causes of infertility (for example, endometriosis).
Treatment

For the treatment of functional tubal infertility, sedatives, tranquilizers, psychotherapy, antispasmodics, blockers of prostaglandin synthesis (naproxen, indomethacin, ibuprofen, acetylsalicylic acid - in the preovulatory period), hydrogen sulfide baths, pulsed ultrasound, electrostimulation of the fallopian tubes are used.
The prognosis with timely therapy is satisfactory.
With tubal infertility of inflammatory genesis, chronic inflammatory processes of the uterine appendages are treated.
With prolonged (more than 2 years) conservative treatment of tubal infertility, dystrophic changes in the fallopian tubes develop, folds of the mucous membrane grow together, connective tissue develops in the muscular and mucous layers, and the receptor apparatus of the fallopian tubes is damaged.
Therefore, timely surgical treatment of tubal infertility is necessary.
An absolute contraindication to surgery is genital tuberculosis. Relative contraindications: the woman's age is over 35 years, the duration of tubal infertility is more than 3 years, frequent exacerbations of a chronic inflammatory process in the uterine appendages and an acute inflammatory process suffered during the previous year, a pronounced adhesion process in the small pelvis, the presence of a large hydrosalpinx, which, when removed, will remain no more than 5 cm of fallopian tubes. For operations on the fallopian tubes, a microsurgical technique is used.
In the postoperative period, resorption therapy is indicated: electrophoresis of zinc and copper, magnetotherapy, ultrasound, enzyme preparations. Within 4 months. after surgery, contraception is recommended, preferably with synthetic progestins.
The pregnancy rate after operations using microsurgical techniques reaches 50%. In some cases, surgical interventions are performed during laparoscopy using an operating laparoscope: dissection of adhesions, coagulation of endometrioid heterotopies, etc.
Prevention of tubal infertility
Prevention of tubal infertility includes the prevention and rational treatment of inflammatory diseases of the genital organs, timely diagnosis and treatment of appendicitis, and early rehabilitation after gynecological operations in young women.
Infertility due to various gynecological diseases

The causes of infertility can be external and internal endometriosis, intrauterine synechiae, malformations of the cervix and uterus, cervicitis, endometritis. With inflammatory diseases of the cervix, its congenital or traumatic (during abortion, childbirth, operations), anatomical changes, as well as with hypoestrogenism and the formation of antibodies to sperm, there may be a violation of the permeability of cervical mucus for spermatozoa, which is detected using the postcoital test, tests for the penetration of sperm into the cervical mucus and the contact of sperm with cervical mucus.
Immunological infertility
Immunological infertility in women is caused by the appearance of antibodies to sperm.
It is diagnosed using tests for compatibility of sperm and cervical mucus, detection of antibodies in blood serum, and cervical mucus.
Therapy of immunological infertility is not sufficiently developed, glucocorticoid drugs are used, which have immunosuppressive and anti-inflammatory properties, the method of artificial insemination with the partner's sperm, injected directly into the uterine cavity, bypassing the cervix.
Post by Karen Willson, gynecologist at Mother and Baby Centre, London, UK
(Updated at Apr 15 / 2024)
Duphaston articles:
Some of the trademarks used in this Web Site appear for identification purposes only.
All orders are reviewed by a licensed physician and pharmacist before being dispensed and shipped.
The statements contained herein are not intended to diagnose, treat, cure or prevent disease. The statements are for informational purposes only and is it not meant to replace the services or recommendations of a physician or qualified health care practitioner. If you have questions about the drugs you are taking, check with your doctor, nurse, or pharmacist.